Combating Non-Alcoholic Fatty Liver Disease (NAFLD)
Because of the definite links between diabetes and liver disease, it’s important that everyone, particularly those already diagnosed with type 2 diabetes, focus on liver health.
What is Non-Alcoholic Fatty Liver Disease? (NAFLD)
There’s always some fat flowing in and out of the liver.
In fact, the liver makes fat, glucose, fructose, and other compounds, and packages fat for distribution throughout the body.
Sometimes, however, the liver can get over-run with fat.
This leads to inflammation, insulin resistance, damage to the liver cells, and can become NAFLD and lead to type 2 diabetes.
The build-up of fat in the liver is a form of “energy toxicity” and comes from obesity, over-consumption of fructose, over-eating, lack of physical activity, and high blood insulin levels.
Fatty liver can be detected through imaging and blood testing. Imaging includes MRI, Ultrasound, and CT scans, measuring the amount of fat in the liver. Blood testing includes what are often termed “liver enzymes”, such as alanine aminotransferase test (ALT), aspartate aminotransferase test (AST), and Gamma glutamyl transferase (GGT).
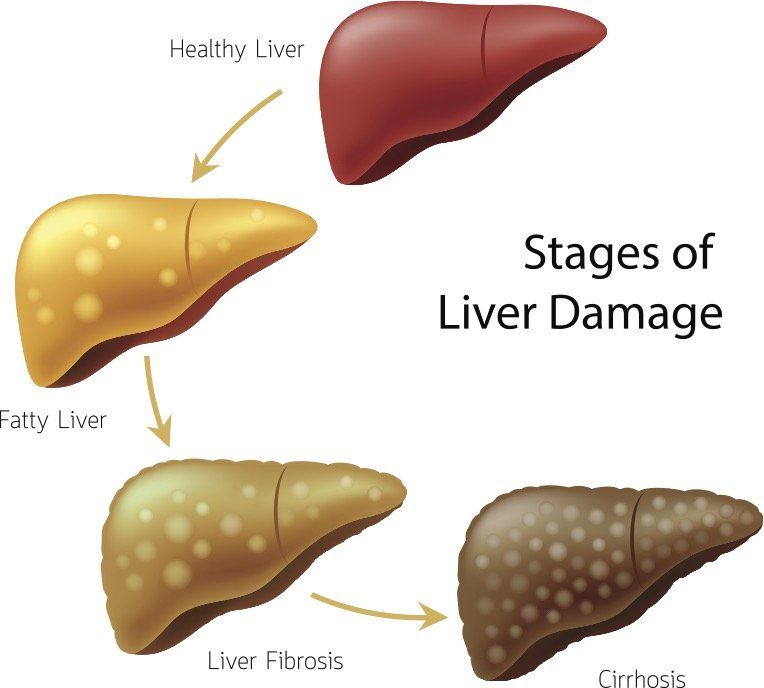
Fatty Liver Disease Progresses Through 4 Stages:
Fat Build Up
Inflammation
Scarring
Permanent Damage
What Causes Non-Alcoholic Fatty Liver Disease? (NAFLD)
Processed Foods
A diet rich in processed and refined carbohydrates, which typically includes a
high amount of fructose, leads to increased fat production and storage in the
liver.
Overeating
When you consume more energy, in the form of fat and carbohydrates, than
you burn, the excess energy can get trapped in the liver, leading to a build-up of fat.
InsulinResistance to the hormone insulin leads to elevated blood levels of insulin.
Since insulin encourages fat storage and suppresses the breakdown of fat,
this can lead to an accumulation of fat in the liver.
Visceral Fat
Some people tend to store more fat around the midsection than others.
Having an “apple shape”, or central adiposity with an elevated waist-to-height
ratio, increases the risk for NAFLD.
Chronic Inflammation
While some inflammation is normal, chronic systemic inflammation from
toxins, gut dysbiosis, poor diet, or infections leads to insulin resistance and
may contribute to NAFLD.
Lack of Physical Activity
Exercise is a great way to burn extra energy, including fat from the body.
Sedentary lifestyles lead to more energy toxicity and a greater risk of fatty
liver.
The Connection between NAFLD and Diabetes
Most people understand the association between consuming large amounts of refined sugar and carbohydrates (as well as processed foods and fake fats), and the development of type 2 diabetes.
Too much sugar causes blood glucose levels to skyrocket, which causes the pancreas to have to pump out high levels of insulin to process that glucose. Over time, our pancreas gets beat up, and our cells become resistant to insulin, and we must support this natural metabolic process through artificial means, like medications and injected insulin. There is evidence showing the development of type 2diabetes may also stem from certain types of sugar’s effect on the liver.

Fructose - Your Livers Enemy
When we talk about sugar, we’re talking about several different molecules:
- Glucose
- Galactose
- Fructose.
Glucose can be metabolized by every cell in the body and, if we don’t get it from our diet, our bodies make it.
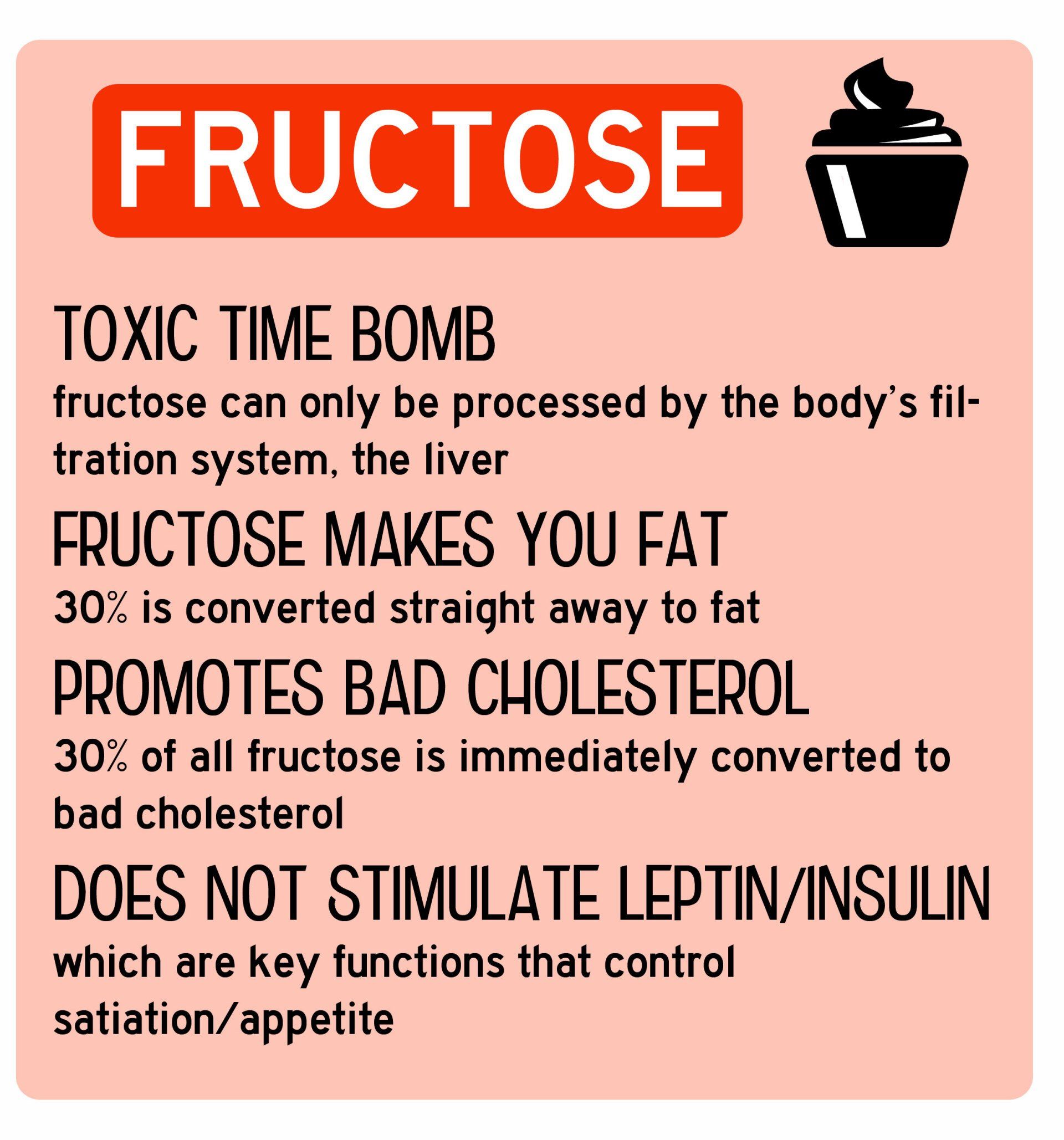
Fructose, however, can only be metabolized by the liver, because only the liver has a transporter for it.
Athletes can generally eat quite a bit of fructose without having any health issues because their livers turn the fructose into glycogen, a storage form of glucose in the liver.
Being very active, athletes would burn through the glycogen making room for more. But those people who aren’t as active… their livers are constantly full of glycogen.
So, what happens when they consume more fructose (easily found in most processed foods)?
The fructose will be turned into fat. Some of the fat is released from the liver and accounts for blood triglycerides, while much of the fat remains in the liver, causing NAFLD.
At the exact same time as your liver is getting fat, it is also becoming insulin resistant. This combination causes elevated insulin throughout your body, leading to obesity, metabolic syndrome, and other diseases.
After some time, the pancreas becomes unable to secrete sufficient insulin to get all that glucose into your cells, and eventually, you are diagnosed with type 2 diabetes.

Symptoms of Non-Alcoholic Fatty Liver Disease (NAFLD)
- Fatigue
- Hormone imbalance
- PMS
- Loss of appetite
- Jaundice
- Allergies
- Bloating and gas
- Heartburn
- Allergies
- Poor sleep quality
- Gallstones or gallbladder problems
- High blood pressure
- Sugar cravings
- Frequent headaches
- Acne or oily skin
- Poor concentration
- Inability to lose weight
- Mood swings
- Bad breath
- Coated tongue
Foods To Help Reverse Non-Alcoholic Fatty Liver Disease (NAFLD).
Grapefruit
Grapefruit is high in vitamin C and other powerful antioxidants and increases the cleansing processes of the liver. Consider incorporating a squeeze of grapefruit or a few drops of grapefruit essential oil in your water first thing in the morning.
Green Tea
Green tea is full of plant antioxidants known as catechins; compounds known to assist liver function. While the actual tea offers many health benefits, the green tea extract is much higher in the helpful catechins.
Leafy Green Vegetables
Leafy greens such as spinach and kale are powerful allies in cleansing the liver. Plus, they’re delicious and versatile because they can be eaten raw, cooked, or juices. Leafy greens can neutralize heavy metals, chemicals and pesticides, allowing your liver to heal and function properly.
Fibre
Increasing fibre can help bind extra fat in the gut, reducing circulating levels of triglyceride and cholesterol. Additionally, 10-20 grams of soluble fibre per day has been shown to improve insulin sensitivity and reduce liver fat.
Olive Oil
The main fat in olive oil in oleic acid, a monounsaturated fat. This type of fat, associated with the Mediterranean diet, has been shown to reduce liver fat and reverse NAFLD. One study published in Diabetes Care found that a diet enriched with monounsaturated fats was associated with a “clinically relevant reduction of hepatic fat content in type 2 diabetic patients independent of an aerobic training program”.
These fats can also be found in avocado, meats, and nuts and seeds.
Coffee
Coffee beans are a good source of caffeic acid, which has been shown to improve fatty liver disease by reducing inflammation and oxidative stress. In fact, studies show that people who drink two or more cups of coffee per day have less risk for NAFLD than those who do not consume caffeine.
Making a change to combat Non-Alcoholic Fatty Liver Disease (NAFLD).
If you’ve been diagnosed with diabetes or are overweight, it’s important to understand the connection between your overall health and the health of your liver. If you want to start really loving your liver, the best things you can do are to clean up your diet (cut out excessive sugars and processed foods), incorporate the foods listed above, and get plenty of exercise.
Have Questions? I've Got Answers
Let's Talk
Simple changes get results. You don't have to live your life always reacting to foods with no energy and low libido.